The intricate relationship between anxiety and addiction forms a complex interplay that significantly influences an individual’s mental and emotional well-being. Anxiety, a prevalent mental health condition, can often serve as both a precursor to substance abuse and a consequence thereof.
Understanding the dynamics between anxiety and addiction is crucial for developing effective interventions and holistic treatment approaches. In this exploration, we delve into the ways in which anxiety and addiction relate, examining how one can exacerbate the other and the intricate pathways that intertwine these two challenging facets of human experience.
Table of Contents
What is Anxiety?
Anxiety is a natural human response to stress or danger. It is a feeling of fear, unease, or worry about future events or uncertain outcomes. While it is normal to experience occasional anxiety, excessive or persistent anxiety that interferes with daily life and functioning may indicate an anxiety disorder.
According to the National Center for Biotechnology Information, anxiety disorders are the most common mental illness in the United States. Approximately 33.7% of U.S. adults will experience an anxiety disorder at some point in their lives.
Anxiety disorders encompass a range of conditions, such as generalized anxiety disorder (GAD), panic disorder, social anxiety disorder, and specific phobias. These disorders can significantly impact a person’s quality of life, relationships, and overall well-being.
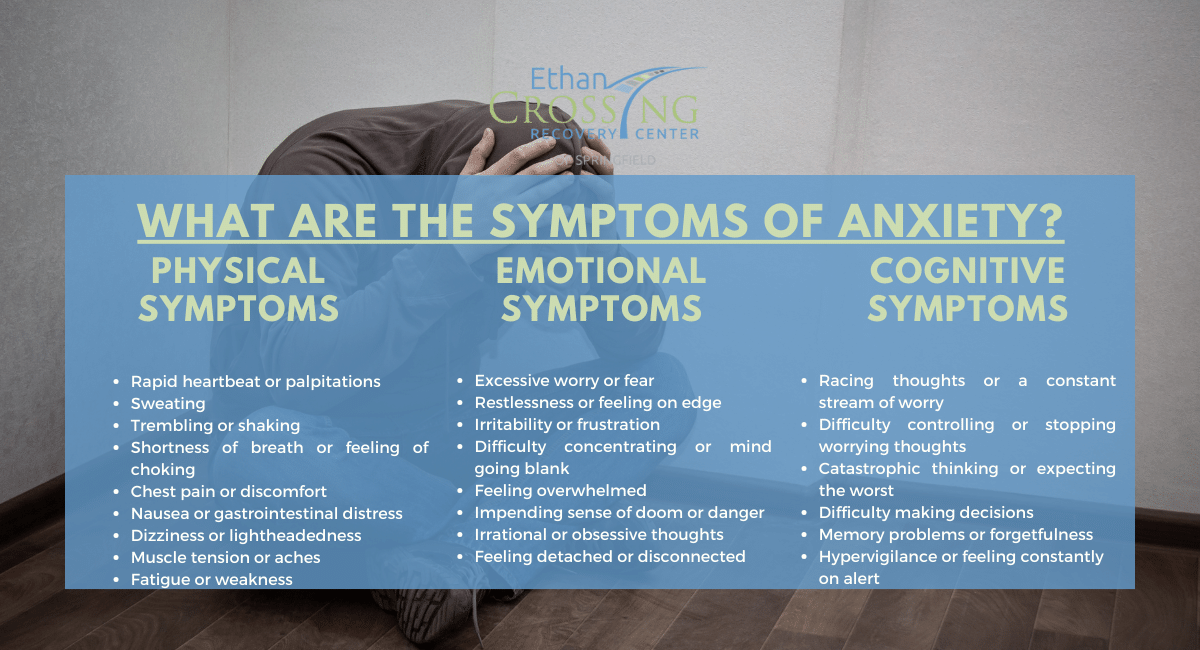
What are the Symptoms of Anxiety?
The symptoms of anxiety can vary from person to person, but they generally involve a combination of physical, emotional, and cognitive manifestations. Here are some common symptoms associated with anxiety:
1. Physical symptoms
- Rapid heartbeat or palpitations
- Sweating
- Trembling or shaking
- Shortness of breath or feeling of choking
- Chest pain or discomfort
- Nausea or gastrointestinal distress
- Dizziness or lightheadedness
- Muscle tension or aches
- Fatigue or weakness
- Insomnia or difficulty sleeping
2. Emotional symptoms
- Excessive worry or fear
- Restlessness or feeling on edge
- Irritability or frustration
- Difficulty concentrating or mind going blank
- Feeling overwhelmed
- Impending sense of doom or danger
- Irrational or obsessive thoughts
- Feeling detached or disconnected
3. Cognitive symptoms
- Racing thoughts or a constant stream of worry
- Difficulty controlling or stopping worrying thoughts
- Catastrophic thinking or expecting the worst
- Difficulty making decisions
- Memory problems or forgetfulness
- Hypervigilance or feeling constantly on alert
Note that experiencing occasional anxiety is normal and can even be helpful in certain situations. However, when anxiety becomes excessive, persistent, and interferes with daily life, it may indicate an anxiety disorder requiring immediate treatment.
What are the Different Types of Anxiety Disorders?
There are several different types of anxiety disorders recognized by mental health professionals. These disorders share common features of excessive and persistent anxiety or fear, but they also have distinct characteristics. The main types of anxiety disorders include:
1. Generalized Anxiety Disorder (GAD)
GAD is characterized by excessive worry and anxiety about everyday life events and situations. People with GAD often find it challenging to control their worry, and their anxiety may be accompanied by physical symptoms like restlessness, fatigue, muscle tension, and difficulty concentrating.
2. Panic Disorder
Panic disorder involves recurrent and unexpected panic attacks, which are intense episodes of fear or discomfort that reach a peak within minutes. Panic attacks are often accompanied by physical symptoms such as a rapid heartbeat, sweating, trembling, shortness of breath, and a sense of impending doom. People with panic disorder may also develop a fear of having future panic attacks, leading to behavioral changes and avoidance of certain situations.
3. Social Anxiety Disorder (Social Phobia)
Social anxiety disorder is characterized by an intense fear of social situations and the fear of being judged or humiliated by others. People with social anxiety disorder may experience significant distress and avoidance of social interactions, which can interfere with their personal and professional lives.
4. Specific Phobias
Specific phobias involve an intense and irrational fear of a specific object, situation, or activity. Common phobias include fear of heights, spiders, flying, or confined spaces. When faced with a phobic stimulus, individuals may experience extreme anxiety and may go to great lengths to avoid the feared object or situation.
5. Obsessive-Compulsive Disorder (OCD)
OCD is characterized by intrusive and unwanted thoughts (obsessions) that lead to repetitive behaviors or mental rituals (compulsions) aimed at reducing anxiety. People with OCD often feel compelled to perform these rituals to alleviate distress, even though they recognize that their thoughts and behaviors are excessive or irrational.
6. Post-Traumatic Stress Disorder (PTSD)
PTSD can develop after experiencing or witnessing a traumatic event. Symptoms may include intrusive memories or flashbacks of the traumatic event, avoidance of reminders of the trauma, negative changes in mood and thinking, and increased arousal or hypervigilance. PTSD can significantly impact daily functioning and quality of life.
Some individuals may experience symptoms that overlap across different anxiety disorders, and it is possible to have more than one anxiety disorder simultaneously. Proper diagnosis and individualized treatment plans are essential for managing anxiety disorders effectively.
What are the Causes and Potential Risks of Anxiety Disorders?
The causes of anxiety disorders are complex and can involve a combination of genetic, environmental, and psychological factors. While it’s not always possible to pinpoint a single cause for an individual’s anxiety disorder, the following factors are believed to contribute to the development of these disorders:
1. Genetics
There is evidence to suggest that anxiety disorders can run in families, indicating a genetic predisposition. Certain genetic variations or inherited traits may increase the likelihood of developing an anxiety disorder.
2. Brain Chemistry and Structure
Imbalances in brain chemicals called neurotransmitters, such as serotonin, norepinephrine, and gamma-aminobutyric acid (GABA), are thought to play a role in anxiety disorders. Additionally, differences in the structure and function of certain brain regions involved in fear and anxiety responses, such as the amygdala and prefrontal cortex, have been observed in individuals with anxiety disorders.
3. Environmental Factors
Traumatic or stressful life experiences, such as physical or emotional abuse, neglect, or the loss of a loved one, can contribute to the development of anxiety disorders. Chronic stress from work, school, relationships, or financial difficulties may also increase the risk.
4. Personality Factors
Certain personality traits, such as being highly self-critical, having low self-esteem, or being prone to perfectionism, may predispose individuals to develop anxiety disorders. Additionally, individuals with a tendency to view the world as threatening or dangerous may be more susceptible to anxiety.
5. Medical Conditions and Substance Abuse
Some medical conditions, such as heart disease, respiratory disorders, or hormonal imbalances, can be associated with anxiety symptoms. Substance abuse, including alcohol and drug misuse, can also contribute to the development or exacerbation of anxiety disorders.
6. Traumatic Events
Exposure to traumatic events, such as natural disasters, accidents, or violence, can increase the risk of developing anxiety disorders, particularly post-traumatic stress disorder (PTSD). Army veterans, for example, may experience PTSD at one point or the other from their experiences in action. Research by the National Center for PTSD suggests that seven out of 100 veterans will have PTSD.
Some other causes of anxiety disorders may include:
- Family History
- Childhood Experiences
- Chronic Medical Conditions
- Substance Withdrawal
- Personality Disorders
- Life Transitions and Major Life Events
- Chronic Stress
- Cultural and Environmental Factors
- Co-occurring Mental Health Conditions
Remember that each individual’s experience with anxiety disorders is unique, and the interplay of these factors can vary.
What is Addiction?
Addiction is a complex and chronic disorder characterized by compulsive and uncontrollable engagement in a substance or behavior despite negative consequences. It is often associated with a physical and psychological dependence on a substance or activity.
Substance addiction typically refers to the excessive and persistent use of substances such as alcohol, tobacco, prescription medications, or illicit drugs. Meanwhile, behavioral addiction involves compulsive engagement in activities such as gambling, gaming, internet use, or shopping. Both substance and behavioral addictions can have profound effects on an individual’s physical and mental health, relationships, and overall functioning.
What are the Symptoms of Addiction?
The symptoms of addiction can vary depending on the specific substance or behavior involved. However, there are common signs and symptoms that are indicative of addiction, regardless of the substance or behavior. These symptoms include:
- Compulsive Engagement: The individual engages in the substance or behavior repeatedly and in larger amounts or for longer durations than intended.
- Loss of Control: The person has difficulty controlling or stopping their substance use or engagement in the behavior, despite attempts to do so.
- Preoccupation: There is a strong preoccupation with obtaining the substance or engaging in the behavior, often spending significant time thinking about it.
- Cravings: There are intense and persistent cravings or urges for the substance or behavior, making it difficult to resist.
- Neglecting Responsibilities: The individual neglects or gives up important social, occupational, or recreational activities in favor of substance use or engaging in addictive behavior.
- Continued Use Despite Consequences: Despite experiencing negative consequences, such as physical health problems, relationship difficulties, financial troubles, or legal issues, the person continues to use the substance or engage in the behavior.
- Withdrawal Symptoms: When the substance use is discontinued or significantly reduced, the person experiences withdrawal symptoms, which can be physical or psychological in nature. These symptoms vary depending on the substance involved.
- Tolerance: Over time, the person requires increasing amounts of the substance or engagement in the behavior to achieve the desired effect. This can indicate the development of tolerance.
- Continued Use Despite Awareness: The individual is aware of the negative consequences and the impact of their substance use or behavior but continues to engage in it regardless.
- Emotional Distress: The person may experience emotional distress, such as irritability, restlessness, or anxiety, when unable to engage in the addictive behavior or access the substance.
The presence of these symptoms alone does not necessarily indicate addiction. A formal diagnosis should be made by a healthcare professional or addiction specialist based on a comprehensive assessment of the individual’s symptoms, behaviors, and circumstances.
What is the Relationship Between Anxiety and Addiction – (Dual-Diagnosis)?
Anxiety and addiction often co-occur and can have a complex relationship. While not everyone with anxiety develops an addiction, and not everyone with an addiction has anxiety, there are several ways in which these two conditions can interact:
1. Self-Medication
Some individuals with anxiety may turn to substances or addictive behaviors as a way to self-medicate and alleviate their anxiety symptoms temporarily. Alcohol, drugs, or certain behaviors like excessive gambling or internet use may provide temporary relief from anxiety. However, this self-medication can lead to a cycle of dependency and addiction.
2. Substance-Induced Anxiety
Substance use, particularly of certain substances like stimulants or hallucinogens, can trigger or worsen anxiety symptoms. The use of substances can disrupt the brain’s natural balance and contribute to anxiety disorders or exacerbate existing anxiety.
3. Anxiety as a Risk Factor
Anxiety disorders, such as generalized anxiety disorder (GAD), social anxiety disorder, or panic disorder, can increase the risk of developing an addiction. The distress and discomfort associated with anxiety may lead individuals to seek relief through substances or addictive behaviors.
4. Common Underlying Factors
Anxiety disorders and addiction can share common underlying risk factors, such as genetic predisposition, neurochemical imbalances, or early-life trauma. These factors can contribute to the development of both conditions or make individuals vulnerable to experiencing both simultaneously.
5. Cycle of Co-Occurrence
Anxiety and addiction can contribute to a self-perpetuating cycle. Anxiety may drive individuals to seek relief through substances or addictive behaviors, and the short-term relief they experience reinforces the association between anxiety relief and the addictive substance or behavior. However, over time, addiction can worsen anxiety symptoms and create additional stressors in an individual’s life, leading to a cycle of escalating anxiety and addiction.
6. Increased Vulnerability to Relapse
Individuals in recovery from addiction who also have anxiety disorders may be at an increased risk of relapse. Anxiety symptoms can trigger cravings or lead to using substances or engaging in addictive behaviors as a coping mechanism to manage anxiety.
It is essential for individuals with co-occurring anxiety and addiction to receive comprehensive and integrated treatment that addresses both conditions simultaneously. This may involve a combination of therapies, such as cognitive-behavioral therapy (CBT), medication management, support groups, and stress management techniques.
What is the Best Treatment for the Co-Occurence of Anxiety and Addiction?
The best treatment for individuals with dual diagnoses of anxiety and addiction typically involves an integrated and comprehensive approach that addresses both conditions simultaneously. The specific treatment plan may vary depending on the severity of symptoms, individual needs, and treatment preferences. Here are some common treatment approaches:
1. Integrated Therapy
Integrated therapy involves combining evidence-based treatments for both anxiety disorders and addiction. This approach recognizes the interconnectedness of the two conditions and aims to address them together. Integrated therapy may include a combination of individual therapy, group therapy, and family therapy.
2. Cognitive-Behavioral Therapy (CBT)
CBT is a widely used therapy that focuses on identifying and modifying unhealthy thought patterns and behaviors. It can be effective for both anxiety and addiction by helping individuals develop healthier coping strategies, manage triggers and cravings, and challenge negative thinking patterns.
3. Medication
Medication may be prescribed to help manage symptoms of anxiety and support addiction recovery. Anti-anxiety medications, such as selective serotonin reuptake inhibitors (SSRIs) or benzodiazepines, may be used to alleviate anxiety symptoms. Medications for addiction, such as medications for opioid or alcohol use disorder, may also be considered in certain cases.
4. Support Groups
Support groups, such as 12-step programs like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA), can provide a supportive and understanding community for individuals in recovery. These groups offer a platform for sharing experiences, receiving guidance, and obtaining ongoing support.
5. Dual-Diagnosis Treatment Programs
Dual-diagnosis treatment programs are specifically designed to address the unique needs of individuals with co-occurring anxiety and addiction. These programs typically offer specialized therapeutic interventions, integrated treatment plans, and a multidisciplinary team of professionals experienced in managing dual-diagnosis cases.
6. Stress Management Techniques
Learning and practicing stress management techniques can be beneficial for managing anxiety and reducing the risk of relapse. Techniques such as mindfulness meditation, deep breathing exercises, physical exercise, and relaxation techniques can help individuals cope with anxiety and reduce the urge to turn to addictive substances or behaviors.
7. Lifestyle Changes
Making positive lifestyle changes can support recovery from both anxiety and addiction. This includes adopting a healthy diet, getting regular exercise, improving sleep patterns, and engaging in activities that promote overall well-being.
Recovery from anxiety and addiction is a journey that requires ongoing support and commitment. With the right treatment and support, individuals can manage their symptoms, reduce the impact of anxiety, and work towards long-term recovery from addiction.
Can drugs and alcohol cause anxiety?
Yes, drugs and alcohol can cause or worsen anxiety symptoms. Stimulants like cocaine and amphetamines can increase arousal and trigger anxiety. Hallucinogens can induce overwhelming experiences leading to anxiety and panic. Alcohol can initially produce calming effects but can lead to rebound anxiety and long-term symptoms. Substance withdrawal can also cause anxiety. Co-occurring anxiety and substance use disorders are common. Seeking professional help is important for managing anxiety and substance use concerns.
What causes anxiety in the brain?
The causes of anxiety in the brain are believed to involve factors such as neurotransmitter imbalances, hyperactivity in the amygdala (the brain’s fear center), dysregulation of the HPA axis (the stress response system), genetic factors, environmental influences, and cognitive processes. These factors interact in complex ways and contribute to the development and experience of anxiety disorders.
What is the connection between anxiety and addiction?
Anxiety and addiction are closely linked, often co-occurring and influencing each other in a complex manner. The relationship between these two conditions can be bidirectional, with anxiety contributing to the development of addiction and addiction worsening anxiety symptoms. Individuals with anxiety may turn to substances or addictive behaviors as a means of self-medication, while substance use can induce or exacerbate anxiety symptoms.
Common underlying factors, such as genetic predisposition and neurochemical imbalances, can increase the risk of developing both anxiety and addiction. The co-occurrence of anxiety and addiction requires a comprehensive and integrated treatment approach that addresses both conditions simultaneously. Integrated therapy, including cognitive-behavioral therapy (CBT), medication management, support groups, and stress management techniques, is often recommended.
Get Help From Anxiety and Addiction
At Ethan Crossing Recovery Center, we understand the intricate relationship between anxiety and addiction, recognizing the unique challenges individuals face when grappling with both conditions. Our dedicated team of professionals is committed to providing comprehensive and compassionate care to those seeking help in overcoming anxiety and addiction.
We offer a tailored approach that integrates evidence-based therapeutic interventions, addressing the root causes of anxiety while fostering a supportive environment for addiction recovery. By combining clinical expertise with personalized treatment plans, we aim to empower individuals on their journey to lasting wellness.