High-functioning depression, also known as persistent depressive disorder (PDD), is a subtype of depression that often goes unnoticed due to individuals maintaining a seemingly successful and productive lifestyle. While they may excel in their careers, maintain relationships, and engage in daily activities, their internal battle with depressive symptoms persists.
This article will explore the signs, symptoms, and treatment options for high-functioning depression. Understanding the unique challenges faced by individuals with high-functioning depression is crucial in recognizing and addressing this often-overlooked mental health condition.
By shedding light on this topic, we hope to promote awareness, encourage early intervention, and provide guidance for effective treatment strategies to support those living with high-functioning depression.
Table of Contents
What is High Functioning Depression?
High-functioning depression, also known as persistent depressive disorder (PDD) or dysthymia, is a subtype of depression where individuals experience chronic depressive symptoms while maintaining a seemingly functional and successful lifestyle.
A good example is a successful CEO who appears to have it all together. They have a thriving career, a loving family, and an active social life. They excel at their job, meet their responsibilities, and engage in social activities with friends and loved ones. However, internally, they battle with persistent feelings of sadness, emptiness, and self-doubt.
Despite their accomplishments, they wake up each morning with a sense of heaviness, struggling to find motivation and joy in their daily life. They constantly question their worth, feel a deep-rooted sense of sadness, and experience a lack of interest or pleasure in activities they used to enjoy. It becomes increasingly challenging for them to concentrate and focus on their tasks, but they manage to maintain a facade of competence and productivity to the outside world.
Although the CEO may appear functional and successful on the surface, their high-functioning depression is a constant presence, affecting their overall well-being and quality of life.
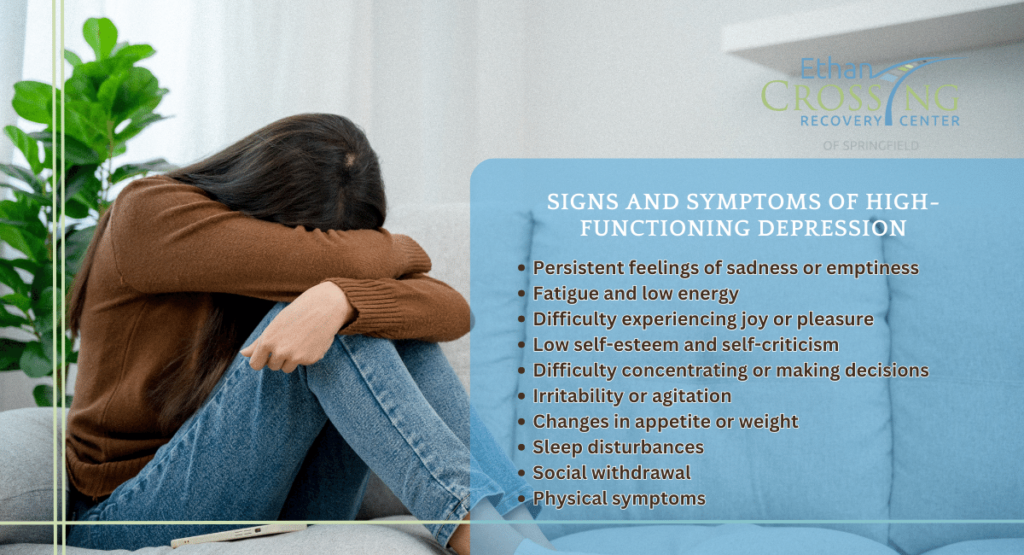
What are the Signs and Symptoms of High-Functioning Depression?
The signs and symptoms of high-functioning depression can vary from person to person, but here are some common indicators to look out for:
- Persistent feelings of sadness or emptiness: Individuals with high-functioning depression may experience a deep and prolonged sense of sadness, even when they appear to be functioning well.
- Fatigue and low energy: Feeling tired and lacking energy despite getting adequate rest is a common symptom. It can make daily tasks and responsibilities feel overwhelming.
- Difficulty experiencing joy or pleasure: A diminished interest or inability to find pleasure in activities that used to be enjoyable is a key symptom. Hobbies, social gatherings, and other previously satisfying experiences may no longer bring the same level of fulfillment.
- Low self-esteem and self-criticism: People with high-functioning depression often have a negative self-image and engage in self-critical thoughts. They may feel unworthy, inadequate, or constantly blame themselves for perceived shortcomings.
- Difficulty concentrating or making decisions: Cognitive difficulties, such as trouble concentrating, making decisions, or remembering details, may be present. This can affect work or academic performance.
- Irritability or agitation: Feelings of irritability, restlessness, or being easily agitated can manifest, even in situations that wouldn’t typically provoke such reactions.
- Changes in appetite or weight: High-functioning depression may lead to changes in appetite, resulting in either weight gain or weight loss. Some individuals may experience emotional eating as a coping mechanism.
- Sleep disturbances: Insomnia, trouble falling asleep, or waking up too early are common sleep disturbances associated with high-functioning depression. Others may experience excessive sleep and find it challenging to get out of bed.
- Social withdrawal: Despite maintaining a high level of functioning, individuals may withdraw from social interactions or isolate themselves due to a lack of energy, interest, or feelings of disconnection.
- Physical symptoms: Symptoms such as headaches, digestive issues, muscle tension, or other unexplained physical discomforts can be present.
It’s important to note that not everyone with high-functioning depression will experience all of these symptoms. Additionally, symptoms may fluctuate in intensity over time. If you or someone you know is exhibiting signs of high-functioning depression, it is advisable to seek professional help from a mental health provider for an accurate diagnosis and proper treatment.
What are the Factors That Contribute to High-Functioning Depression
Several factors can contribute to high-functioning depression, also known as persistent depressive disorder (PDD). It’s important to note that these factors can interact and vary from person to person. Here are some common contributors:
1. Biological Factors
Imbalances in brain chemicals, such as serotonin, dopamine, and norepinephrine, are thought to play a role in depression. Genetic factors may also increase the vulnerability to developing high-functioning depression, as there can be a hereditary predisposition to mood disorders.
2. Environmental Factors
Stressful life events, such as trauma, loss, or chronic stress, can contribute to the development and persistence of high-functioning depression. Ongoing challenges in personal or professional life, financial difficulties, or relationship problems can also contribute to the condition.
3. Personality Traits
Certain personality traits may increase the risk of high-functioning depression. Perfectionism, self-criticism, excessive need for control, or a tendency to internalize emotions can make individuals more susceptible to depressive symptoms, even while maintaining a high level of functioning.
4. Childhood Adversity
Experiences of abuse, neglect, or other adverse childhood experiences can have long-lasting effects on mental health. Childhood trauma or adverse experiences can increase the risk of developing high-functioning depression later in life.
5. Cognitive Factors
Negative thinking patterns, distorted beliefs about oneself or the world, and a tendency to ruminate or dwell on negative experiences can contribute to high-functioning depression. These cognitive factors can perpetuate and intensify depressive symptoms.
6. Lack of Social Support
Limited social support and a lack of healthy relationships or a strong support network can contribute to high-functioning depression. Feelings of isolation or a perceived lack of understanding or validation from others can impact one’s emotional well-being.
7. Coping Mechanisms
Unhealthy coping mechanisms, such as substance abuse, excessive work, or avoidance of emotions, may provide temporary relief but can contribute to the persistence of depressive symptoms in the long term.
Understanding these contributing factors can help inform treatment approaches and strategies for managing high-functioning depression effectively.
How is High-Functioning Depression Diagnosed?
Diagnosing high-functioning depression, or persistent depressive disorder (PDD), typically involves a comprehensive evaluation by a mental health professional. Here’s an overview of the diagnostic process:
1. Initial Assessment
A mental health provider, such as a psychiatrist, psychologist, or licensed therapist, will conduct an initial assessment. This may involve a discussion of your symptoms, medical history, and any relevant personal or family history of mental health conditions.
2. Diagnostic Criteria
The mental health professional will refer to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) published by the American Psychiatric Association. They will evaluate whether your symptoms align with the specific criteria for high-functioning depression (PDD).
3. Symptom Duration
To meet the diagnostic criteria for high-functioning depression, symptoms must be present for most days, for at least two years (or one year for children and adolescents). During this time, there may be periods of milder or more severe symptoms.
4. Functional Impairment
The mental health professional will assess whether your symptoms are causing significant distress or impairment in various areas of your life, such as work, relationships, or social functioning. Despite maintaining a relatively high level of functioning, individuals with high-functioning depression may still experience challenges and difficulties.
5. Differential Diagnosis
The mental health provider will consider other possible explanations for your symptoms and rule out other mental health conditions or medical conditions that may present with similar symptoms. This helps ensure an accurate diagnosis.
6. Collaboration
To gather a comprehensive understanding of your condition, the mental health professional may collaborate with other healthcare providers involved in your care, such as primary care physicians or specialists, if necessary.
What are the Treatment Options for High-Functioning Depression?
The treatment options for high-functioning depression, or persistent depressive disorder (PDD), typically involve a combination of psychotherapy, medication, and self-care strategies. The specific approach will depend on the individual’s needs, preferences, and the severity of their symptoms. Below are some common treatment options:
1. Psychotherapy (Talk Therapy)
- Cognitive Behavioral Therapy (CBT): This form of therapy focuses on identifying and changing negative thought patterns and behaviors that contribute to depression. It helps individuals develop healthier coping strategies and more positive ways of thinking.
- Interpersonal Therapy (IPT): IPT focuses on improving relationships and social functioning, as difficulties in interpersonal relationships can contribute to depressive symptoms.
- Psychodynamic Therapy: This therapy explores the underlying emotional and psychological factors that contribute to depression, helping individuals gain insight into their thoughts, feelings, and past experiences.
2. Medication
Antidepressant Medications: Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), or other types of antidepressants may be prescribed to help alleviate depressive symptoms. It’s important to work closely with a psychiatrist or prescribing healthcare provider to find the medication and dosage that works best for you.
3. Self-Care Strategies
- Regular Exercise: Engaging in physical activity can boost mood and improve overall well-being. Aim for regular exercise, even if it’s light or moderate-intensity activities like walking, yoga, or swimming.
- Healthy Lifestyle: Prioritize a balanced diet, adequate sleep, and stress management techniques to support your mental health.
- Stress Reduction: Incorporate stress reduction techniques such as mindfulness, meditation, deep breathing exercises, or engaging in hobbies and activities that bring you joy.
- Establishing Supportive Relationships: Seek the support of loved ones, friends, or support groups. Sharing your experiences and feelings with trusted individuals can provide emotional support.
4. Supportive Services
- Support Groups: Joining a support group for depression can provide a sense of community and understanding. It allows individuals to share experiences, gather insights, and learn from others who are going through similar challenges.
- Case Management: In more severe cases or when additional support is needed, a mental health professional or case manager can help coordinate treatment, provide resources, and assist with navigating the healthcare system.
Remember that treatment for high-functioning depression is individualized, and what works for one person may not work for another. It’s recommended to work closely with mental health professionals who can tailor a treatment plan to your specific needs and monitor your progress.
Is High-Functioning Depression Hereditary?
Research suggests that there may be a genetic component to high-functioning depression, indicating that it can have a hereditary or familial predisposition. However, the exact genetic mechanisms and specific genes involved in high-functioning depression are not yet fully understood.
Family and twin studies have shown that individuals with a family history of depression, including high-functioning depression, have an increased risk of developing the condition themselves. However, it’s important to note that genetics alone do not determine whether someone will develop high-functioning depression. Environmental factors, life experiences, and other non-genetic factors also play a significant role.
Are You or Someone You Love Battling High-Functioning Depression?
Are you or someone you love battling high-functioning depression? At Ethan Crossing, we understand the unique challenges that come with maintaining a high level of functioning while dealing with internal struggles.
Our dedicated team of mental health professionals is here to provide compassionate support and evidence-based treatment specifically tailored to individuals with high-functioning depression. Through a combination of therapy, medication management, and holistic approaches, we aim to help you regain your well-being and find sustainable strategies to thrive in all aspects of life.
Take the first step towards healing by reaching out to Ethan Crossing today.