Delirium tremens (DT) is a challenging and distressing condition that some individuals experience when going through alcohol withdrawal. It is a life-threatening condition requiring immediate medical attention.
The symptoms of delirium tremens can include severe agitation, confusion, disorientation, hallucinations (typically visual), tremors, rapid heartbeat, fever, sweating, and changes in blood pressure. These symptoms can be extremely distressing and may lead to a state of medical emergency if not properly managed.
The primary cause of delirium tremens is alcohol withdrawal following a period of heavy and prolonged alcohol use, with risk factors including chronic alcohol abuse, abrupt cessation or significant reduction of alcohol intake, individual sensitivity, previous episodes of delirium tremens, and co-occurring medical conditions.
Table of Contents
What is Delirium Tremens?
Delirium tremens (DT) is a severe and potentially life-threatening condition that can occur as a result of alcohol withdrawal. According to Wikipedia, the term is a Latin phrase meaning “shaking frenzy.” It is characterized by a rapid onset of symptoms that typically appear within 48 to 96 hours after a person has stopped or significantly reduced their alcohol intake, particularly after a period of heavy and prolonged alcohol use. Delirium tremens most commonly affects individuals with a history of alcohol abuse or dependence.
Delirium tremens is considered a medical emergency, and immediate medical attention is crucial. Treatment typically involves providing supportive care, including administration of fluids, medications to manage symptoms and prevent complications (such as benzodiazepines to reduce agitation and seizures), and close monitoring of vital signs.
It’s important to note that delirium tremens is a serious condition, and individuals experiencing alcohol withdrawal should seek medical assistance to ensure their safety and receive appropriate care.
Delirium tremens is relatively uncommon compared to general alcohol withdrawal syndrome. It is estimated to occur in about 5% of individuals who experience alcohol withdrawal. However, the risk of developing delirium tremens increases among individuals with a history of heavy, long-term alcohol use.
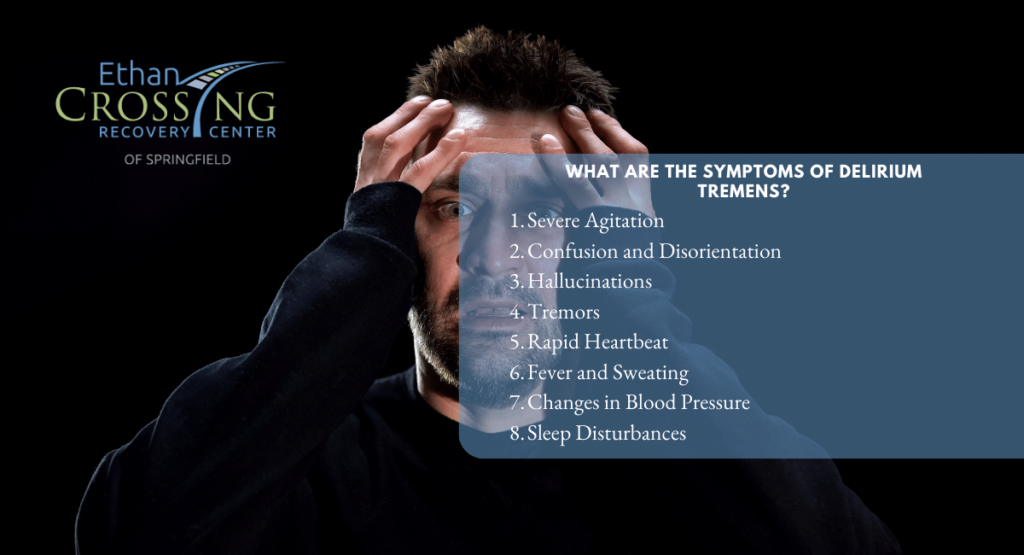
What are the Symptoms of Delirium Tremens?
The symptoms of delirium tremens (DT) can vary in severity and typically occur within 48 to 96 hours after a person has stopped or significantly reduced their alcohol intake. Common symptoms of DT include:
- Severe Agitation: Intense restlessness, irritability, and an inability to calm down.
- Confusion and Disorientation: Difficulty focusing, thinking clearly, and maintaining a coherent conversation. Disorientation to time, place, and person may also be present.
- Hallucinations: Visual hallucinations are a hallmark symptom of DT. These hallucinations are typically vivid and may involve seeing objects, people, or animals that are not actually present.
- Tremors: Shaking or trembling of the hands, arms, or other parts of the body. These tremors can be severe and may worsen with movement or stress.
- Rapid Heartbeat: An abnormally fast heart rate (tachycardia) that can be accompanied by palpitations or a pounding sensation in the chest.
- Fever and Sweating: Increased body temperature and profuse sweating, which can contribute to dehydration.
- Changes in Blood Pressure: Blood pressure fluctuations may occur, leading to either elevated or decreased blood pressure.
- Sleep Disturbances: Insomnia or disrupted sleep patterns, with difficulty falling asleep or staying asleep.
If you or someone you know is experiencing symptoms of DT, it is crucial to seek professional help promptly. Medical intervention is essential to manage the symptoms, prevent complications, and ensure the safety and well-being of the individual.
What are the Causes and Risk Factors of Delirium Tremens?
The primary cause of delirium tremens is alcohol withdrawal, specifically the sudden cessation or significant reduction of alcohol consumption after a period of heavy and prolonged use. The exact mechanisms underlying the development of DT are not fully understood, but it is believed to involve complex neurochemical and physiological changes in the brain.
Chronic and excessive alcohol consumption affects the central nervous system, leading to adaptations and dependence. When alcohol intake is abruptly stopped or reduced, the brain undergoes a rebound effect, as it tries to restore normal functioning without the depressant effects of alcohol. According to the Centers for Disease Control and Prevention, a heavy drinker is someone who consumes as much as 15 drinks per week.
The specific risk factors contributing to the development of delirium tremens include:
- Heavy and Prolonged Alcohol Use: Long-term, excessive alcohol consumption alters the brain’s chemical balance, leading to tolerance and dependence.
- Alcohol Withdrawal Syndrome: Abrupt cessation or a significant reduction in alcohol intake triggers alcohol withdrawal syndrome, which can manifest as a range of symptoms, including delirium tremens.
- Individual Sensitivity: Some individuals may be more susceptible to developing DT due to genetic factors or individual variations in brain chemistry.
- Previous Episodes: Individuals who have experienced delirium tremens during previous alcohol withdrawal episodes are at a higher risk of recurrence.
- Co-occurring Medical Conditions: Pre-existing medical conditions, such as liver disease or a history of seizures, can increase the likelihood of developing DT.
Note that not everyone who experiences alcohol withdrawal will develop delirium tremens. The individual’s overall health, the extent and duration of alcohol use, and other individual factors contribute to the risk.
How is Delirium Tremens Diagnosed?
Delirium tremens (DT) is diagnosed through a combination of medical assessment, symptom evaluation, observation, and monitoring, including:
- Clinical evaluation
- Assessment of withdrawal severity
- Observation and monitoring of symptoms
- Laboratory tests
- Differential diagnosis
Healthcare professionals conduct a thorough examination, assess the severity of alcohol withdrawal symptoms, closely monitor the individual, perform necessary laboratory tests, and consider other potential causes to rule out alternative explanations.
Accurate diagnosis is crucial in order to provide appropriate medical care and intervention for individuals experiencing DT. Do not attempt to self-diagnose or self-treat DT as it is a serious condition requiring expert evaluation and management.
What are the Treatment Options for Delirium Tremens?
The treatment of delirium tremens (DT) typically involves a combination of medical interventions and supportive care. The primary goals of treatment are to manage symptoms, prevent complications, ensure the safety of the individual, and address the underlying alcohol use disorder. Here are some common treatment options for DT:
- Hospitalization: Most individuals with DT require hospitalization to receive specialized medical care and close monitoring.
- Medications: Benzodiazepines, such as diazepam (Valium) or lorazepam (Ativan), are commonly used to alleviate symptoms, control agitation, prevent seizures, and promote relaxation.
- Fluid and Electrolyte Management: Intravenous fluids are administered to address dehydration and correct electrolyte imbalances caused by excessive alcohol consumption and withdrawal.
- Nutritional Support: Adequate nutrition is essential, and individuals may receive intravenous or oral nutritional supplementation to address deficiencies and promote recovery.
- Supportive Care: Creating a calm and supportive environment is crucial. Providing reassurance, comfort, and safety measures can help manage anxiety and reduce distress.
- Treatment for Alcohol Use Disorder: Once stabilized, individuals are encouraged to seek treatment for their underlying alcohol use disorder, which may involve counseling, therapy, support groups, and rehabilitation programs.
In addition to other treatments, Acamprosate may be used and continued in the long term to reduce the risk of relapse, while status epilepticus is typically treated in the standard manner. Providing a well-lit room can be beneficial as it may help alleviate hallucinations experienced by individuals.
Alcoholic beverages are also sometimes prescribed as a treatment option, although this approach is not universally endorsed. Additionally, high doses of thiamine, often administered intravenously, are commonly recommended. It is important to note that the treatment of delirium tremens should be conducted under the supervision of medical professionals.
What is Drug-Induced Delirium?
Drug-induced delirium, also known as substance-induced delirium, refers to a temporary state of confusion, disorientation, and cognitive impairment that is caused by the use or withdrawal of certain medications or substances. It is characterized by a rapid onset of symptoms and can affect attention, memory, and consciousness.
Several drugs and classes of substances have the potential to induce delirium. Some examples include:
- Sedatives and Hypnotics: Benzodiazepines (such as lorazepam or diazepam), barbiturates, and other medications used for sleep or anxiety disorders.
- Anticholinergic Medications: Certain antihistamines, tricyclic antidepressants, medications for overactive bladder, and some antipsychotic drugs.
- Opioids: Strong opioid pain medications, such as morphine or oxycodone, especially when used in high doses or in individuals who are not tolerant to opioids.
- Anticonvulsant Medications: Some antiepileptic drugs, such as phenytoin or carbamazepine, particularly when used in high doses or in combination with other medications.
- Intoxicating Substances: Alcohol, hallucinogens, cannabis (particularly in high doses or in susceptible individuals), and certain illicit drugs.
Note that drug-induced delirium can occur in individuals of any age, but it is more prevalent in older adults who may be more vulnerable to the effects of medications and have multiple medical conditions.
What are Some Common Complications that may Happen During an Episode of Delirium Tremens?
During an episode of delirium tremens (DT), several complications can arise, some of which include:
- Dehydration and electrolyte imbalances
- Cardiovascular disturbances
- Respiratory problems
- Seizures
- Injury and self-Harm
- Hyperthermia
- Psychiatric complications
- Alcohol-related liver disease
- Alcoholic cardiomyopathy
- Alcoholic neuropathy
- Wernicke-Korsakoff syndrome
It is important to note that the complications of DT can be life-threatening. Prompt medical attention and appropriate management are critical to address these complications, ensure the safety of the individual, and prevent further harm.
Get Help at Ethan Crossing
Delirium tremens (DT) is a severe condition that occurs during alcohol withdrawal. It requires hospitalization for specialized care and close monitoring. Treatment involves medications to alleviate symptoms, fluid management, nutritional support, and a supportive environment.
If you or someone you know is struggling with depression, We at Ethan Crossing are available to help. We have experienced therapists and psychologists that offer personalized counseling sessions, often incorporating effective approaches like cognitive-behavioral therapy, to support groups where you can share experiences and find communal support. Contact us today to start your journey to freedom.